With the kind of diseases, including cancer, blood disorders, or immune deficiencies, considered serious, there transpiring hope for patients thanks to several advanced treatment options available before us today in the field of medicine. Now, therapies under the very fanciful could be cell therapy and bone marrow transplant (BMT). While both aim at healing the body on a cellular level, thus, like a liver transplant treatment that fixes any organ failure, this is where the similarity ends. Thus, a good understanding of these two will empower patients and caregivers for an educated decision in their manner of treatment.
What Is Cell Therapy?
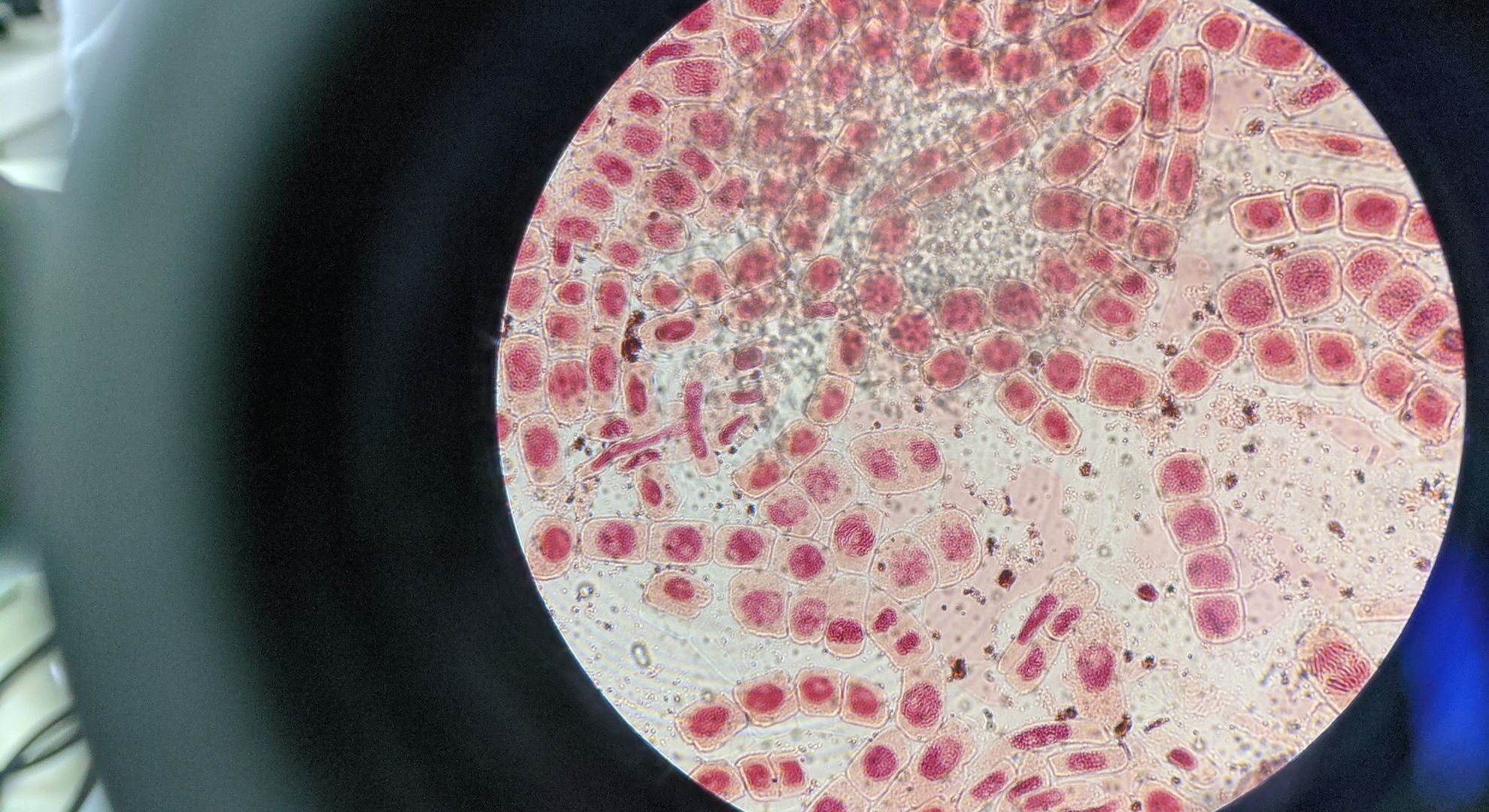
Cell therapy is a term applied to a method in which living cells are implanted into the body to treat or even heal damaged tissues and cellular functions. These cells might be picked up from the patient (autologous) or obtained from a donor (allogeneic), sometimes they might be enhanced or genetically modified prior to being injected back into the human body.
CAR-T cell therapy is probably the best known method for modern cell therapies. T-cells are collected from a patient and genetically reprogrammed to seek out and kill cancer cells, and then the modified cells are reinfused into that patient. CAR-T therapies have been shown to have highly encouraging results especially for blood cancers such as leukemias and lymphomas.
Key Features of Cell Therapy
- Designed for specific diseases or conditions
- Can use autotransplantation of patient cells, or the cells of a donor
- Often genetically modified (like CAR-T)
- Mostly employed in clinical trials or in highly specialized cancer cases
- May not always require complete immune suppression
What Is a Bone Marrow Transplant?
A Bone Marrow Transplant (BMT), also known as a hematopoietic stem cell transplant, is a well-established treatment in which stem cells are used to replace diseased or damaged bone marrow. This is frequently done following high-dose chemotherapy or radiation, which has a significant effect on bone marrow. The main types of BMT are:
Autologous Transplant: The patient’s own stem cells are used for the transplant
Allogeneic Transplant: Stem cells from a donor; either a family member, matched donor, or an unrelated matched donor
BMT is primarily utilized to treat blood cancers such as leukemia, lymphoma and multiple myeloma, but also to treat genetic disorders such as sickle cell anemia and thalassemia.
Key Features of Bone Marrow Transplant
- Totally replaces the whole immune system or bone marrow
- Multiple pre-transplant requirements, most of which are chemotherapy or radiation
- Might including a higher risk of complications like graft-versus-host disease (GVHD)
- Usually means a longer stay in the hospital and takes longer to recover
- Allogenic transplants require someone else who is matched closely enough to be a donor.
Cell Therapy vs. Bone Marrow Transplant: A Side-by-Side Comparison
| Feature | Cell Therapy | Bone Marrow Transplant |
| Purpose | Target specific cell functions | Replace diseased bone marrow |
| Procedure | Often outpatient or short hospital stay | Requires hospital stay and immune suppression |
| Risks | Lower, but may include cytokine release syndrome | Higher, including GVHD and infection |
| Personalization | Highly customized (e.g., CAR-T) | Based on donor matching |
| Availability | Limited to specialized centers | Widely available in cancer treatment centers |
| Recovery | Typically quicker | Longer and more intensive recovery |
So, Which One Is Better?
There isn’t a one-size-fits-all answer. The best treatment depends on:
- The specific disease being treated
- The overall health of the patient
- The goals of treatment
Cell therapy is quickly becoming a better option for particular cancers when traditional chemotherapy has failed. It is often more cholinergic and has less likelihood of side effects. Bone marrow transplant is still the standard of care for many blood cancers and genetic diseases, with a proven track record of decades of efficacy.
In some advanced treatment plans, both therapies can be utilized in conjunction with each other, that is, a BMT may be performed first, followed by cell therapy to build upon or maintain its effectiveness.
Conclusion
In the way that a liver transplant can provide an opportunity for new life to someone suffering from end-stage organ failure, cell therapy and bone marrow transplants can provide a fresh start to people with serious blood and immune system disorders. While similar, cell therapy and bone marrow transplant serve different purposes, have different options, and each has different benefits and risks.
To read more free article ( Click Here )